We only get a precious few minutes to give our Rheumatologists a rundown of our autoimmune disease symptoms and potential triggers, much less thoroughly discuss treatment options. Making the most of the limited time can make the difference in creating the most appropriate treatment plan for you.
You can do a few things beforehand and during your appointments to effectively communicate with your doctor and get the care you need to live fully with an autoimmune disease.
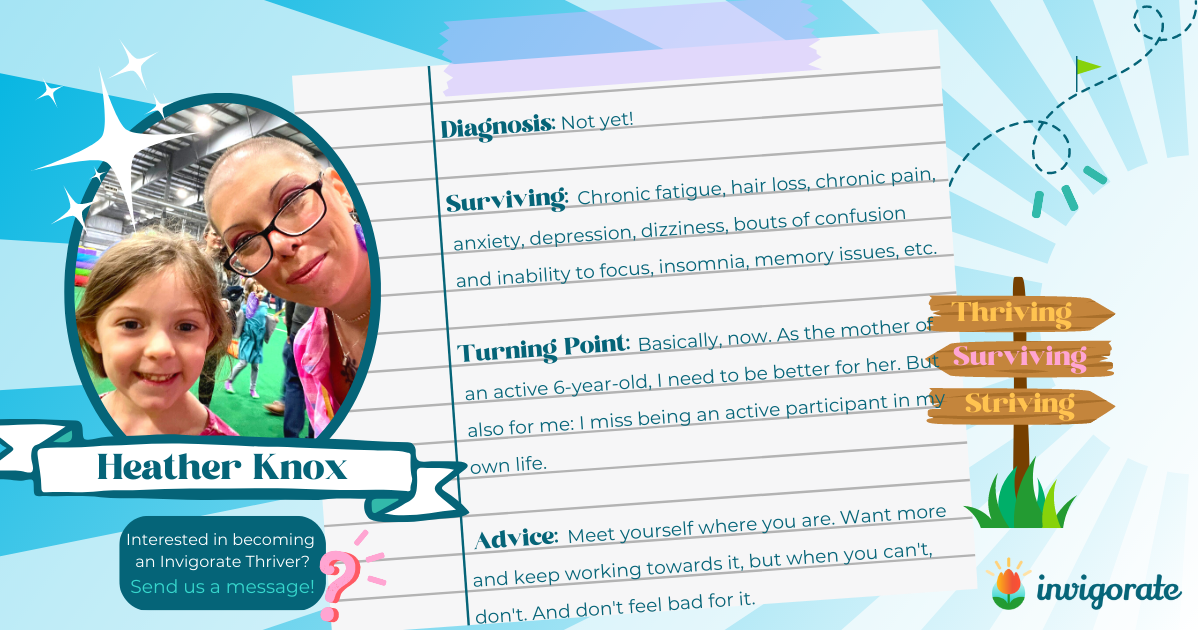
The best place to start is to describe your symptoms precisely. Invigorate Ambassador and Co-Host of the Invigorate Podcast, Chris Burton’s tip: Cut to the chase and give them just the facts. There’s not enough time to tell about your symptoms like you’re talking to a friend.
In this blog, we’ll provide
- Why and how noting and tracking symptoms can improve communication with your Rheumatologist and care team
- 8 questions to consider when tracking and discussing your symptoms
- 5 questions to consider asking your provider during your appointment
How to Get to the Facts: Tracking Symptoms for Better Understanding & Communication With Your Healthcare Team
When dealing with complex diseases and symptoms, recalling and accurately communicating your experiences to healthcare providers can be challenging. That’s why tracking your symptoms daily is a valuable practice that can provide you with a clearer understanding of your condition.
- Clearing the Fog: Symptoms of certain conditions, such as chronic pain or autoimmune diseases, can cause brain fog and make it difficult to remember specific details about how you felt in the past. By tracking your symptoms daily, you create a reliable reference point that helps overcome the challenges of memory recall.
- Identifying Patterns: Tracking allows you to identify patterns and triggers for your symptoms. By noting what you were doing, eating, or exposed to when symptoms occur, you may discover connections that can help pinpoint the underlying causes. This knowledge can assist your healthcare provider in developing a more targeted treatment plan.
- Assessing Progress: Regularly tracking your symptoms enables you to monitor changes over time. You’ll be able to observe whether your symptoms are improving, worsening, or remaining stable. This information is invaluable in evaluating the effectiveness of treatments and interventions.
- Facilitating Effective Communication: A documented record of your symptoms ensures clear and accurate communication with healthcare providers. You can share your tracked data during appointments, which helps your provider understand your condition comprehensively and make informed decisions about your care.
To effectively track your symptoms, consider these options:
Before you head into your appointment, review your symptoms log, make notes, and identify the key points to communicate with your provider. Consider the following questions to help you get started!
Here are 8 questions to consider when discussing your symptoms:
- When did the pain start? What were you doing when it started?
Knowing the onset of your pain can provide valuable insights into its potential causes. Was it a gradual onset or sudden? Did it coincide with an injury or specific activity? Recognizing the trigger can assist your healthcare provider in determining the underlying issue. - What does it feel like — sharp, dull, throbbing, achy, tender?
Describing the quality of your pain can offer additional clues about its nature. Is it a sharp, stabbing sensation or a persistent ache? Does it throb or feel tender to the touch? Providing these details helps your healthcare provider narrow down possible diagnoses. - How severe is the pain on a scale of 1 to 10?
Quantifying the intensity of your pain on a scale of 1 to 10 helps your healthcare provider gauge the severity and assess the impact on your daily life. Being honest and specific is essential, as this information guides treatment decisions. - How has it changed over the last few days or weeks?
Tracking changes in your pain over time is crucial. Did it worsen or improve? Has it spread to other areas? Documenting these developments can aid in diagnosing the condition and evaluating the effectiveness of interventions. - Does anything help the pain, such as over-the-counter (OTC) pain or anti-inflammatory medication or exercise?
Informing your healthcare provider about any measures that temporarily alleviate your pain is essential. It could be using over-the-counter pain relievers, anti-inflammatory medications, or specific exercises. This insight assists in determining what approaches may be practical for managing your symptoms. - How does the pain affect your daily routine?
Understanding how pain impacts your daily activities allows your healthcare provider to comprehend the overall impact on your life. Does it limit mobility, interfere with work, or disrupt sleep? Describing these effects helps tailor treatment plans to address your specific needs. - Is it worse when you get up in the morning?
Morning stiffness and increased pain upon waking can occur in many conditions, such as arthritis or musculoskeletal issues. Noting whether your pain is more pronounced in the morning provides valuable information for diagnosis and treatment recommendations. - Do you have any other symptoms that may seem related?
Pain can often be accompanied by other symptoms that may seem unrelated but could offer additional diagnostic clues—for example, fatigue, sleep disturbances, mood changes, or digestive issues. A comprehensive overview of your symptoms ensures your healthcare provider has a holistic understanding of your condition.
Open communication and an accurate description of your symptoms are crucial to receiving the most appropriate care. Take note of your experiences, be proactive in seeking medical advice, and work collaboratively with your healthcare provider to find the best strategies for managing and alleviating your pain.
How to Get More From Your Provider – 5 Questions to consider asking your provider during your appointment:
- I’m in pain; should I use the joint/muscle or rest it?
Understanding whether rest or activity is the best approach for managing your pain is crucial. In some cases, gentle movement and exercise can promote healing and reduce discomfort. However, rest may be necessary in other situations to prevent further injury. Your healthcare provider can provide personalized advice based on your specific condition. - How do I treat the pain? (Ice? Heat? Pain relievers?)
Understanding the most effective treatment options for your pain is essential. Inquire about appropriate methods, such as applying ice or heat to the affected area. Ice can help reduce inflammation, while heat can ease muscle tension. Your healthcare provider may also recommend over-the-counter or prescription pain relievers to alleviate your symptoms. - Are there other things I can do to feel better?
Beyond conventional treatments, ask your healthcare provider about alternative therapies or complementary approaches that may help manage your pain. These could include physical therapy, acupuncture, massage, or mindfulness techniques. Exploring these options can provide you with a comprehensive pain management plan. - Should I change my diet?
Diet plays a significant role in overall health, including managing pain and inflammation. Inquire if there are any dietary changes or modifications that may be beneficial for your specific condition. Your healthcare provider may recommend an anti-inflammatory diet rich in fruits, vegetables, whole grains, and healthy fats while limiting processed foods and sugary drinks. - Are there vitamins or supplements I could take to help reduce inflammation?
Certain vitamins and supplements have shown potential in reducing inflammation and supporting overall health. Ask your healthcare provider if any specific supplements may benefit your condition. Omega-3 fatty acids, turmeric, ginger, and vitamin D are among the supplements studied for their anti-inflammatory properties.
Remember, these questions are a starting point for a productive conversation with your healthcare provider. Every individual’s situation is unique, and your provider will be able to offer personalized advice based on your medical history, symptoms, and diagnosis. You can work together to develop an effective pain management plan by actively engaging in dialogue and seeking guidance.
Invigorate Founder Karin Wagner and Brand Ambassador Baddest Chaplain Chris Burton, co-host a special podcast episode discussing how to Make the Most of Medical Appointments – Preparing for Your Appointment & Questions to Ask Your Care Team.
Let’s figure it out together, my friends.
Keep dancing,
Karin
Resources: Free Tools to Get More out of Medical Appointments
- Medication List downloadable PDF
- Medication Tracker downloadable PDF
- Sjogren’s Tracker mobile app
- Arthritis Tracker mobile app
- Find more Invigorate Resources at https://invigorateyourjourney.com/manage-autoimmune-disease-flares/
Sources
- Cleveland Clinic – 15 Chronic Pain Management Questions to Ask Your Doctor
- Arthritis Foundation – www.arthritis.org
- YouTube Tedx talk on The 6 Sources of Influence.
- Stanford Health Care – https://stanfordhealthcare.org/medical-conditions/brain-and-nerves/chronic-pain/symptoms.html
- Staff Care – https://www.staffcare.com/locum-tenens-blog/advice/which-physicians-spend-most-time-with-patients/Rheumatology Advisor – https://www.rheumatologyadvisor.com/home/topics/rheumatoid-arthritis/5-best-apps-for-rheumatoid-arthritis/
 Karin W
Karin W 






































 Karin W
Karin W