Welcome back, friends! We’re glad you’re here.
I’m Karin Wagner, and I’ve been on a challenging journey with Lupus for 15 years. Throughout this time, I’ve had the privilege of meeting incredible people who have inspired me, including my Invigorate podcast co-host, the Baddest Chaplain Chris Burton.
We have shared experiences facing various Lupus challenges and are now helping others navigate through their autoimmune journeys.
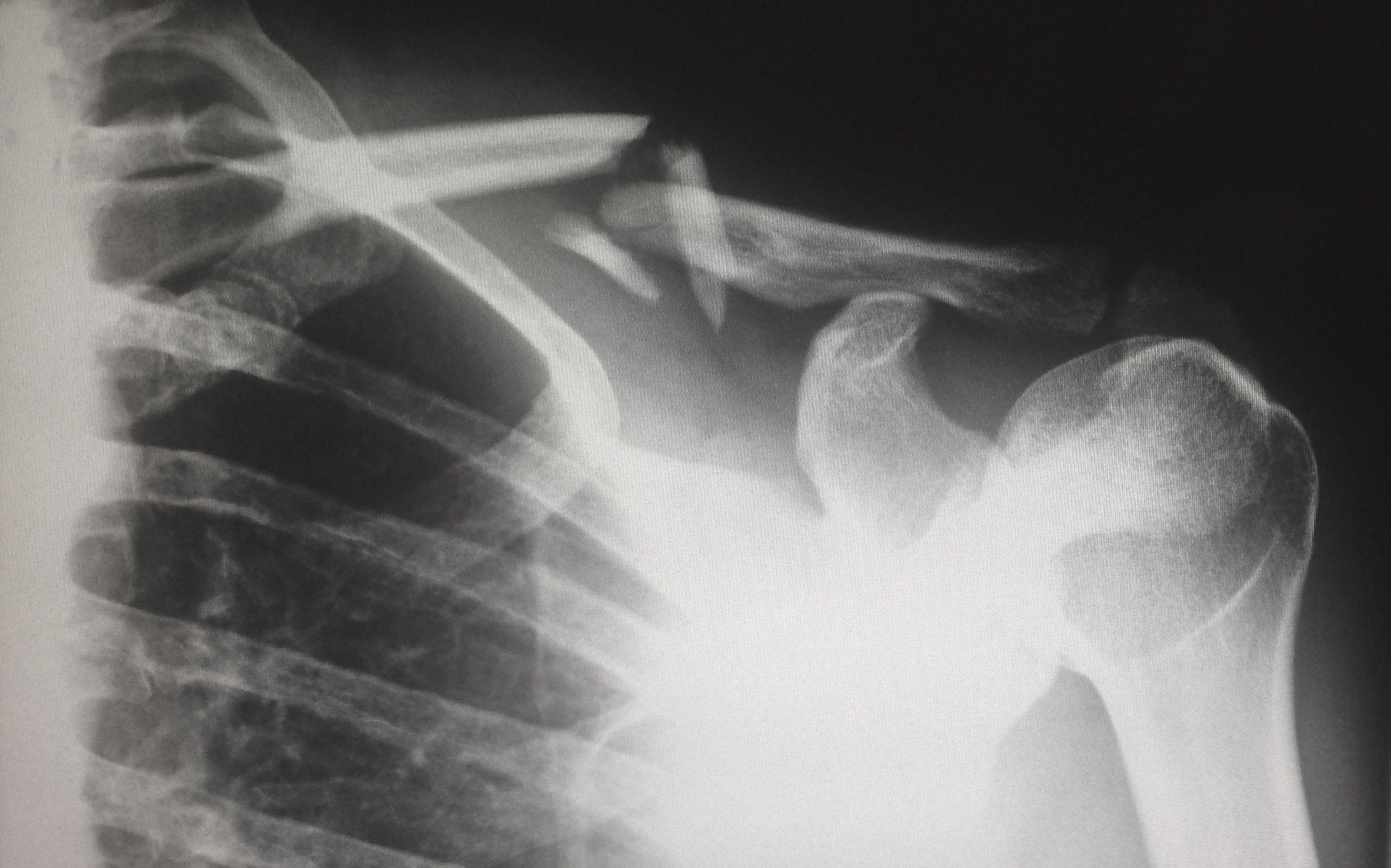
Today, we’re talking about a common yet incredibly painful symptom of autoimmune diseases – joint pain and inflammation. For those of us living with these conditions, it’s a daily struggle that can impact every aspect of our lives. The good news is that there are ways to manage this pain and inflammation and improve our overall quality of life.
Understanding the Pain: Joint Pain in Autoimmune Diseases
Joint pain, as many of us know all too well, is a relentless companion in our journey with autoimmune diseases. Joints can swell, stiffen, and become inflamed, making even the simplest tasks feel like monumental challenges. It can affect any joint, from knees and elbows to hands and shoulders.
The pain is often excruciating, making daily life a relentless uphill battle. It’s not just physical; it’s emotionally taxing, too. But today, we want to offer hope and practical advice. We want you to know that you’re not alone, and there are strategies to help you manage this pain and regain control over your life.
The Link Between Inflammation and Joint Pain
Before we dive into those strategies, it’s crucial to understand the link between inflammation and joint pain. Inflammation is the body’s natural response to injury or infection. However, in the case of autoimmune diseases, our immune system mistakenly triggers inflammation without any apparent injury or infection.
This chronic inflammation can cause damage to the joints and surrounding tissues, leading to pain and stiffness. Addressing inflammation is, therefore, key to reducing joint pain and improving overall health.
Dietary Strategies for Reducing Joint Pain
One of the most powerful tools in our arsenal for managing joint pain and inflammation is our diet. What we eat can either exacerbate or alleviate our symptoms.
In my experience, eliminating refined carbs and dairy has been a game-changer. These are often inflammatory culprits. Sugar, refined carbohydrates, and unhealthy fats can contribute to inflammation.
On the flip side, certain foods have anti-inflammatory properties. Incorporating these into your diet can make a significant difference. Foods rich in antioxidants and omega-3 fatty acids can help reduce inflammation. Think leafy greens, fatty fish, and berries.
Supplements for Relief
In addition to dietary changes and exercise, supplements can be a powerful ally in your battle against inflammation.
Turmeric and Ginger: Nature’s Anti-Inflammatory Duo
Turmeric is a bright orange spice, well-known for its powerful anti-inflammatory properties. It contains an active compound called curcumin, which has been extensively studied for its potential to reduce inflammation in the body. Curcumin works by blocking specific molecules that trigger inflammation, providing relief from joint pain and stiffness.

Ginger is another natural remedy that complements turmeric beautifully. It contains gingerol, an active ingredient with potent anti-inflammatory and antioxidant effects. Much like turmeric, ginger can help reduce joint pain and inflammation by inhibiting the same inflammatory pathways.
Both turmeric and ginger are easy to incorporate into your daily routine. You can add them to your cooking, brew them as teas, or find them in supplement form at your local health store. However, before starting any new supplement, it’s always a good idea to consult your healthcare provider to ensure it’s safe and appropriate for your needs.
Vitamin D: The Sunshine Vitamin
Vitamin D is often referred to as the “sunshine vitamin” because our skin can produce it when exposed to sunlight. This essential nutrient is not only vital for bone health but also plays a role in reducing inflammation.
Research has shown that vitamin D can help regulate the immune system and reduce inflammation in the body. Vitamin D deficiency is associated with an increased risk of autoimmune diseases, including Lupus. Ensuring adequate vitamin D levels through a combination of safe sun exposure and supplementation can be a valuable part of your inflammation management plan.
B Vitamins: Building Blocks of Health
The B vitamins, including B1 (thiamine), B2 (riboflavin), B3 (niacin), B5 (pantothenic acid), B6 (pyridoxine), B7 (biotin), B9 (folate), and B12 (cobalamin), are essential for various bodily functions, including immune system regulation. They can also play a role in reducing inflammation.
Supplements can be valuable to your inflammation management plan when living with autoimmune diseases. Turmeric and ginger, with their natural anti-inflammatory properties, can offer relief from joint pain and stiffness. Vitamin D, the sunshine vitamin, helps regulate the immune system and reduce inflammation. B vitamins, the building blocks of health, have shown promise in managing autoimmune disease symptoms, including inflammation.
However, it’s crucial to remember that supplements are not a one-size-fits-all solution. What works for one person may not work for another, and individual needs can vary significantly. Therefore, always consult with your healthcare provider before incorporating new supplements into your routine. They can help determine the right approach to address your unique situation and provide guidance on the most suitable supplements and dosages for you.
Exercise: The Power of Movement
When dealing with joint pain and inflammation caused by autoimmune diseases, the idea of exercise might seem counterintuitive. After all, moving when you’re in pain doesn’t sound appealing. However, regular exercise, even in the form of gentle activities like stretching and walking, can be a game-changer in your journey to manage these challenging symptoms.
Improving Joint Mobility
I can’t stress enough how essential exercise has been for me in managing my Lupus symptoms. While it might seem daunting at first, I’ve found that even gentle movements can have a significant impact on my joint mobility.
Autoimmune diseases can cause stiffness and decreased range of motion in your joints. Regular exercise helps to counteract this by increasing flexibility and promoting better joint mobility. When you incorporate movement into your daily routine, you’re essentially giving your joints a workout, which can help prevent them from becoming overly stiff and painful.
Strengthening the Muscles Around Your Joints
In addition to improving joint mobility, exercise also strengthens the muscles around your joints. These muscles act as a natural support system for your joints, helping to distribute the workload more evenly and reduce the strain on the affected joints.
It’s important to start slowly and gently, especially if you’re new to exercise or dealing with a flare-up. Begin with simple stretches and range-of-motion exercises, and gradually work your way up to more challenging routines. The goal is to find a balance between keeping your joints mobile without causing excessive pain or strain.
Building a Supportive Exercise Routine
Creating a supportive exercise routine involves a few key considerations:
1. Consult Your Healthcare Provider: Before starting any new exercise regimen, it’s important to consult your rheumatologist or healthcare provider. They can help you tailor a program to your specific needs and ensure it’s safe for your condition.
2. Find What Works for You: Not all exercises are created equal, and what works for one person may not work for another. The key is to find an activity that you enjoy and can stick with. This could be yoga, Pilates, Tai Chi, or even gentle walks.
3. Listen to Your Body: Pay close attention to your body’s signals. If you experience pain during or after exercise, it’s crucial to adjust your routine or consult your healthcare provider for guidance. The goal is to feel better, not worse.
4. Set Realistic Goals: Understand that your exercise routine may need to be adapted during flare-ups or on particularly challenging days. Be flexible with your goals, and remember that any movement is better than none.
5. Consistency Is Key: Consistency is essential when it comes to exercise. Even when you’re not feeling your best, doing some gentle stretching or taking a short walk can make a big difference in the long run.
Remember, your journey is unique, and there’s no one-size-fits-all approach to exercise. The most crucial step is to start. Begin with simple, gentle movements, and gradually build from there. Over time, you’ll find that exercise can become one of your most effective tools in managing joint pain and inflammation.
Managing Stress: The Mind-Body Connection
In the realm of autoimmune diseases, stress is often an unwelcome and relentless companion. It’s not just a mental burden; it can significantly worsen inflammation and pain in the body. Understanding and managing the mind-body connection is essential to regain control over your life.
The Impact of Stress on Inflammation
Stress can be a relentless presence for people with autoimmune diseases and chronic illnesses. When stress levels rise, symptoms tend to intensify. It’s a shared experience among those with autoimmune diseases.
When you’re stressed, your body produces hormones like cortisol and adrenaline, which are part of the “fight or flight” response. These hormones can trigger and exacerbate inflammation in the body. For those of us already dealing with chronic inflammation, this stress-induced response can be especially problematic.
Stress can also affect how we perceive pain. When we’re stressed, our pain tolerance tends to decrease, making the pain we experience feel even more intense. Finding ways to manage stress is crucial. One method that has proven incredibly helpful is meditation.
Meditation: A Calming Practice
Meditation involves focusing on a particular object, thought, or activity to train attention and awareness and achieve a mentally clear, emotionally calm, and stable state.
Meditation can be a transformative practice that reduces stress and helps you become more attuned to your body. It’s about creating a mental space where you can let go of worries, fears, and anxieties, even if just for a few minutes each day.
One technique that works well for many people is called diaphragmatic breathing. It involves taking slow, deep breaths by expanding your diaphragm. Inhale for a count of four, hold for four and exhale for four. This simple practice can have a remarkable impact on your stress levels and overall well-being.
Deep Breathing: A Simple Yet Powerful Tool
Deep breathing is another fantastic technique for managing stress. It’s a simple yet powerful tool that can be done anywhere and anytime.
When you practice deep breathing, you’re essentially sending a signal to your brain that it’s time to relax. This results in a lower heart rate, reduced blood pressure, and a sense of calm and relaxation.
Therapy: Seeking Professional Guidance
In some cases, stress may become overwhelming, and it can be beneficial to seek therapy. Therapists can provide valuable support and guidance in managing stress, which, in turn, helps reduce inflammation and pain.
Therapy offers a safe space to explore your feelings and develop coping strategies. It’s not a sign of weakness but a step toward taking control of your mental and emotional well-being.
There are various therapeutic approaches, including cognitive-behavioral therapy (CBT), which helps change negative thought patterns, and mindfulness-based therapies that promote living in the present moment. Finding the right therapist and approach that suits you is essential.
Reclaiming Control
Autoimmune diseases, joint pain, and inflammation may be part of your journey, but they don’t have to define your life. Managing stress effectively is a critical aspect of this process. By practicing meditation, deep breathing, and seeking therapy when needed, you can reclaim control over your well-being.
Remember, the mind-body connection is a powerful one. When you address stress and its impact on inflammation, you’re not only improving your mental and emotional health but also reducing the physical burden on your body.
Practical Tips for Daily Life
Living with joint pain and inflammation can be challenging, but there are practical tactics you can incorporate to ease symptoms.
Heat and Cold Therapy: One of the most accessible and effective ways to alleviate pain is by applying heat or cold to the affected area. Consult with your doctor to determine the best method for your symptoms. Heat increases blood flow and relaxes tense muscles, while cold therapy can help numb the area and reduce swelling.
Assistive Devices: If joint pain hampers your ability to perform daily tasks, consider using assistive devices. Canes, walkers, or jar openers might not be glamorous, but they can provide much-needed support and alleviate pressure on your joints.
Taking Breaks: Taking regular breaks is crucial if your daily activities involve repetitive motions that exacerbate your pain. Rest and stretch your joints to reduce strain and prevent further inflammation.
Getting Enough Rest: Rest is essential for managing pain and inflammation. It allows your body to repair and rejuvenate. Make sure to prioritize getting enough sleep each night.
It’s important to remember that managing joint pain and inflammation is a journey unique to each individual. While these tips can provide relief, it’s essential to consult with a rheumatologist for a personalized treatment plan.
When to Seek Medical Help
Sometimes, despite our best efforts, our symptoms may intensify or interfere with our daily lives. That’s when it’s crucial to seek medical help.
Rheumatologists are vital in developing individualized treatment plans based on your condition and symptoms. They consider factors such as the severity of inflammation, joint damage, and overall health to determine the most appropriate course of action.
In some cases, your rheumatologist may refer you to other healthcare professionals, like physical therapists, occupational therapists, or pain management specialists, who can provide additional support and therapies to help manage joint pain and inflammation.
Regular monitoring and follow-up with your rheumatologist is essential. They’ll help you adjust your treatment plan as needed and guide lifestyle modifications, exercise routines, and self-care strategies, all aimed at improving your overall well-being.
Consulting with a rheumatologist for personalized advice and treatment options is crucial, but remember that staying on top of inflammation at home can also make a significant difference.
Embracing Hope and Relief
Living with an autoimmune disease, joint pain, and inflammation can significantly impact your quality of life. But with the right strategies, the proper support, and the right mindset, you can reduce pain and inflammation. You can regain control of your symptoms and live a higher quality of life.
Remember, you’re not alone on this journey. We understand and care. We’re here to support you, to share our experiences, and to offer hope for a brighter, pain-free tomorrow. Together, we can invigorate your journey and make every step easier. Thank you for joining us today, and we’ll be back with more soon.
Karin
Resources
- Mindfulness Breathing Techniques
- Recipes and Nutrition
- Exercise Resources
- Manage Flare

 Karin W
Karin W